Sperm Test Spermiogram
Other Name:
Sperm Analysis , Sperm Count , Semen Analysis, Spermiogram
Official Name:
Spermiogram
Other Related Tests:
Anti Sperm Antibody Test, ASA, FSH, LH, Prolactin, Urinalysis, Sperm DNA Damage Test, Sperm Mar Test, Sperm DNA Fragmentation, Sperm Culture, Sperm Fish
Why Have a Sperm Test?
As part of the infertility test, it is investigated after a vasectomy (tying the sperm ducts) if your partner has difficulty conceiving or to determine whether a reproductive health surgery has been successful.
When should a sperm test be done?
It can be considered for control purposes about three months after having a fertility problem or having a vasectomy (connecting the sperm ducts). Sperm volume reductions during ejaculation, painful or painful ejaculation.
Which Sample Is Required For Sperm Test?
Sperm sample collected in a clean, wide-mouthed container provided by the laboratory; It is often collected at the testing site, but sometimes under special circumstances, it must be given at home in a container provided by a laboratory and quickly delivered to the laboratory for analysis.
Is Sperm Test Preparation Necessary?
For Sperm Test, avoid having sex or masturbation 2-5 days before sample collection; Follow the given instructions carefully. If there is an involuntary ejaculation during sleep, the diet should be started from the beginning.
Sperm Test How to use
A semen analysis is done to determine if a man is infertile (infertility) – it cannot make a woman pregnant. Sperm analysis consists of a series of tests that evaluate the quality and quantity of sperm, as well as the sperm and the fluid containing them. The test, along with other infertility tests, can be used to help determine why a couple is not able to conceive (conceive) and guide decisions about infertility treatment.
Semen analysis can also be used to determine if sperm is present in the semen after a man has had a vasectomy (tying the sperm ducts); this is a surgical procedure that prevents sperm from being released in the ejaculate. This surgery is considered a permanent method of birth control (99.9%) when performed successfully.
When is a sperm test required?
Semen (sperm) analysis /Sperm Test is requested when a urologist or gynecologist doctor thinks that a man or a couple may have fertility problems. Infertility is typically diagnosed when a couple has been trying to conceive for 12 months without success.
To determine fertility, a sperm analysis should be performed on at least two samples collected at intervals of 15 to 25 days. Sperm count and semen consistency can vary from day to day, and some conditions can affect sperm motility.
and may temporarily affect their numbers.
When a Sperm Test analysis shows abnormal findings, the test is repeated at intervals determined by the laboratory specialist. Again, it should be at least 2-3 days after fasting.
A shorter version of a Sperm Test analysis, a Sperm Test, is typically ordered approximately 3 months after a vasectomy (tying the sperm ducts) to confirm the success of the procedure, and the sperm is found in the semen sample. It can be repeated as many times as necessary until no longer visible.
What Does the Sperm Test Result Mean?
Sperm Test control after vasectomy (connecting sperm ducts) surgery: Couples can be weaned using other birth control methods when there is no rare non-motile sperm in the sperm or sperm. If sperm is present in the semen, the man and his partner should take precautions to prevent pregnancy. The test can be repeated until there are no more motile sperm in the sperm samples.
Infertility test: In a man’s fertility evaluation, every aspect of the semen analysis and the findings as a whole are fully evaluated. Semen from a man can vary from sample to sample. Abnormal results in a sample may not indicate the cause of infertility and multiple samples may need to be tested before a diagnosis can be made.
- Volume – the typical volume of collected sperm is 2 to 5-6 milliliters (about one tablespoon) of fluid per ejaculation. Decreased semen volume indicates less sperm, which reduces opportunities for successful fertilization and subsequent pregnancy. Excess seminal fluid (total sperm volume) can dilute sperm concentration.
- Viscosity – semen should initially be mushy and then liquefy within 15 to 30 minutes. If this doesn’t happen, it can hinder sperm movement.
- Sperm concentration (also called sperm count or sperm density) – this is measured in millions of sperm per milliliter of semen. Normal is at least 20 million or more sperm per milliliter, and the total ejaculate volume is 80 million or more sperm. Fewer sperm and/or a lower sperm concentration can reduce fertility.
- Mobility – percentage of motile sperm in a sample; rated by speed and direction traveled. An hour after discharge it should be at least 50% mobile, it will move in a straight line at good speed. Sperm progression is graded from zero (quiescent) to 4, 3-4 representing good motility. If less than half of the sperm are motile, a blot is used to determine the percentage of dead sperm. This is called sperm viability test.
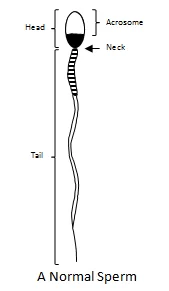
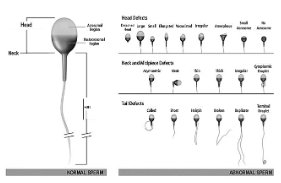
- Morphology – size, shape and appearance of sperm cells; The analysis evaluates the structure of the sperm. More than 50% of the cells examined should be normal in size, shape, and length. The more abnormal sperm present, the higher the probability of infertility. Abnormal forms may include faulty heads, midsections, tails, and immature forms. You can search the web for an image of a normal sperm.
- In a normal sperm:
- A smooth, oval-shaped head with a length of 5-6 micrometers and a width of 2.5-3.5 micrometers
- (less than the size of a pinpoint)
- A good looking head (acrosome) covering 40% to 70% of the sperm head
- No visible abnormalities of the neck, midpiece or tail
- There should be no liquid droplets larger than half the size of the sperm head in the sperm head
How Can a Sperm Be Abnormal?
Sperm can have multiple defects, as seen in the image below and to the right. These can affect the head, neck or tail area.

So Your Sperm Morphology Is Low – Should You Worry?
Low sperm morphology (the shape or physical appearance of sperm is not something you want to hear after a semen analysis, but it happens more often than you think.
It is quite common for fertile men to have a low percentage of ideally shaped sperm; however, when the proportion of ideally formed sperm is significantly reduced, the chances of being fertile are lower. While there is a definite trend between normal-appearing sperm and fertility potential, this does not mean that a man with a sperm analysis result of 0% normal-shaped sperm cannot father a child as a child; Millions!
Defects in the shape of the sperm neck or tail can affect movement; Defects in the sperm head can affect the sperm’s ability to attach to and fertilize the egg. When evaluated using strict World Health Organization (WHO) criteria, the morphology result is simply a marker of sperm function, which affects the sperm’s chances of fertilizing an egg. It is important to remember that if an egg is fertilized with an abnormal ‘looking’ sperm, it does not increase the likelihood of potential birth defects in any resulting child.
Semen Analysis Evaluates Your Sperm
If you are actively trying to conceive with your partner the only way to determine what type of sperm you are producing is semen analysis. Given that a semen analysis is a highly non-invasive procedure, this is often one of the first tests your Fertility Specialist recommends during fertility research.
Sperm morphology is the only thing we evaluate in a semen analysis. It also depends on the semen volume, pH, the number of sperm in a sample (concentration), how fast the sperm swim (motility), and whether the sperm are piling up together (usually due to sperm-producing antibodies after trauma involving the testicles or certain diseases). In general, higher numbers of abnormally shaped sperm are associated with other irregularities of the sperm such as low sperm count or motility.
What is Normal Shaped Sperm?

In a normal sperm:
- A smooth, oval-shaped head (smaller than the size of a pinpoint) 5-6 micrometers long and 2.5-3.5 micrometers wide
- A well-defined cap (acrosome) covering 40% to 70% of the sperm head
- No visible abnormalities of the neck, midpiece or tail
- No liquid droplets larger than half the size of the sperm head
- Semen pH – should be between 7.2 and 7.8. A pH of 8.0 or higher may indicate an infection, while a pH of less than 7.0 indicates urine contamination or a blockage in the ejaculatory ducts.
- The fructose concentration should be greater than 150 milligrams per deciliter of semen.
- White blood cells – There should be less than 1 million white blood cells per milliliter.
- Sperm agglutination – this occurs when sperm adhere specifically and consistently (head to head, tail to tail, etc.) indicating the presence of antisperm antibodies. Non-specific clumping of sperm may be due to bacterial infection or tissue contamination.
Is there anything I can do to improve my sperm shape?Research has shown an association between abnormal sperm shape and the use of tobacco, alcohol, and caffeine. While trying for pregnancy, you should not use tobacco or recreational drugs, and limit your consumption of alcohol and caffeine. These substances can affect the quality of sperm DNA (the material that carries your genes). At the same time, it is important to maintain a healthy weight and make sure you eat a balanced diet, because it also has an effect on sperm. We recommend using propolis as it is recommended to improve reproductive health. Also multi-vitamin supplements, however, any changes in diet and lifestyle can take up to 3 months for noticeable increases in sperm quality to occur, as this is roughly the length of the sperm cycle. Sometimes changes (such as DNA integrity) are routinely required. ://www.labistanbul.com.tr/sperm-testi-2.html”>semen analysis cannot be evaluated. Instead, it is clearly visible in tests that look at sperm DNA integrity, such as the sperm DNA damage test.
- The time the couple is trying to conceive
- Frequency and timing of intercourse
- age of wife
- cause of infertility
These factors, together with the result of the semen analysis, tell the infertility specialist for which condition he or she recommends the most appropriate treatment.
Is there anything else I should know?
While abnormal results reduce the likelihood of conception, some couples with poor results on infertility tests may continue to think with or without assistance, and those with seemingly good results may experience difficulties.
Various factors can affect sperm count or other semen analysis values, including the use of alcohol, tobacco, caffeine, many recreational and prescription drugs, and some herbal medicines as is known on the market.
What is Tested in Sperm Analysis?
A literal semen (sperm) analysis measures the amount and quality of semen released during sexual ejaculation. It evaluates the moving cells with a microscope called both the liquid part called semen or seminal fluid and the sperm cell. This test is generally used to evaluate male infertility. A shorter version of this test checks for the presence of sperm in the semen a few months after a man has had a vasectomy (canal tying) to determine if the surgery was successful.
Semen is a viscous, whitish opaque liquid containing sperm and products from several glands. It is quite thick during ejaculation, but thins or liquefies within 10 to 30 minutes. Sperm are reproductive cells that have a head, body, and tail in semen and contain one copy of each chromosome (all of the male genes). Sperm are motile, normally they move through the semen. In a woman’s body, thanks to this feature, the females go to their eggs and fuse, resulting in fertilization. Each semen sample is 1.5 to 5.5 milliliters (about one tablespoon) of fluid, containing at least 20 million sperm per milliliter and containing varying amounts of fructose (sugar), buffers, coagulants, lubricants, and enzymes to support. sperm and the fertilization process.
A typical semen analysis measures:
- Semen volume
- Viscosity – semen consistency or fluidity
- Sperm count – total sperm count
- Sperm concentration (density) – number of sperm per semen volume
- Sperm motility – how strongly and evenly the sperm can move in percentage
- Number or percentage (morphology) of normal and abnormal (defective) sperm in terms of size and shape
- Coagulation and liquefaction – how long does it take for semen to turn from thick to liquid
- Fructose – sugar in semen that gives energy to sperm
- pH – measures acidity
- Immature sperm count
- Number of leukocyte (BK) cells (cells indicating infection)
Additional testing may be done if the sperm count is low, if the sperm show decreased motility or abnormal morphology, or if the seminal fluid is found to be abnormal. These additional tests can affect fertility such as the presence of sperm antibodies, abnormal hormone levels (FSH, LH, prolactin), excessive white blood cell count, and Klinefelter syndrome. It can help detect abnormalities such as genetic testing for conditions that may affect cystic fibrosis or other chromosomal abnormality.
In some cases, imaging tests such as ultrasound, CAT scan, or MRI may be required. A testicular biopsy may also be needed. Sometimes if a couple wants to store sperm for future pregnancies, a test called cryosurvival is done to see how well the semen will hold for long-term storage.
How to collect sample for testing
Sperm control after vasectomy: The semen sample is collected in a clean, wide-mouth container provided by the laboratory.
Infertility assessment: Most laboratories require samples to be collected on site because sperm must be examined within 60 minutes of ejaculation to maintain the quality of the sample.
Semen is collected in a special area through self-stimulation. Some men, for religious or other reasons, may wish to collect sperm during sex using a condom. In this case, the healthcare professional should provide the condom or sheath, as lubricated condoms can affect test results.
Sperm are very temperature sensitive. If collection is done at home, the sample should be kept at body temperature (37°C) by keeping it next to the body during transport. It should not be left at room temperature for a long time and should not be stored in the refrigerator.
After ejaculation, sperm motility decreases; Therefore, timing and temperature are crucial to obtaining accurate results. If the sample is weak, repeat testing may be necessary.
NOTE: If passing medical tests makes you or someone you care about anxious, embarrassed or difficult to cope with, you may want to consider coming to our lab for help: Coping with Test Pain, Discomfort and Anxiety, Tips for Blood Testing, Tips for Helping Children with Medical Tests, and Seniors You can get Tips for Helping with Medical Tests from our expert.
Is any test preparation necessary to ensure the quality of the sample?
For infertility testing: Avoid ejaculation for 2 to 5 days before sample collection to give sperm a chance to replenish. Longer periods of abstinence may result in greater sperm volume but reduced sperm motility. You may also be asked to avoid alcohol consumption for several days before the test. Follow the given instructions.
After Vasectomy: Men may be advised to ejaculate regularly every 3-4 days to clear sperm from the reproductive tract more quickly.
The Operation in Our Laboratory;
Before taking Sperm Test, it is necessary to abstain from sexual intercourse for 2 to 5 days. There should be no sexual ejaculation (sleeping or masturbation) for 2-5 days by any means. If it has happened, the diet should be started again before the Sperm Test.
Alcohol, drugs or cigarettes should not be consumed during sexual abstinence. Since these substances affect the sperm count and movement, the Sperm Test misleads the result.
In our Şişli and Kadıköy branches, the Sperm Test is performed with the Kruger method. You do not need to make an appointment to take the Sperm Test, it is sufficient to arrive 3 hours before our closing time.
Samples are accepted between 08:30 and 17:00 on weekdays, Saturday: 08:30 – 13:00. The lab is closed on Sundays
WE HAVE A DVD MOVIE WATCHING ROOM IN OUR LABORATORIES.
There are special sampling rooms in our laboratories for Sperm Test in our Şişli and Kadıköy branches. It is possible to watch DVD while giving samples. You can also bring your own DVD.
During the Sperm Test, sperm shape (morphology) characteristics are examined after a special staining, and the fertility capacity of the sperm sample is determined. Since many factors such as smoking, alcohol, heat, drugs and infections affect sperm production, the analysis of abnormal samples should be repeated two or three times with an interval of one month. If a fertility problem is detected in the sperm analysis, further examination of the man is carried out in terms of physical and hormonal aspects.
Sperm production cycle is repeated every 2-3 months. In other words, a sperm produced will be secreted into the semen after 2-3 months. Likewise, harmful factors that the person encounters or useful drugs used for treatment can also affect sperm production at the end of 3 months. This process should be kept in mind when evaluating the Sperm Test results.
What are the Terms in Explanations and Reports for Abnormal Sperm Test?
* Here is the Sperm Dictionary:
- Aspermia: No Sperm Volume
- Acrosome : The head of the sperm after the tail
- Asthenozoospermia: Sperm Motility < 40%
- Azospermia: Sample No Sperm Cells
- Globozoospermia:headlessround-headed sperm
- Hematospermia: Red blood cells (erythrocytes) in semen
- Hyperspermia: Semen volume> 5.5 ml
- Hyposspermia: Semen volume < 2 ml
- Necrozospermia: Lifeless (“dead”) sperm
- Oligoasthenozoospermia: intensity < 8 million sperm / ml.
- Oligozoospermia: The sperm count is less than 20 million / ml.
- Polyzoospermia: Exceptionally high sperm concentration
- Pyospermia: Leukocytes (germ-fighting cells) in semen
- Teratozoospermia: 40% of sperm is formed abnormally
To get more detailed information about sperm test, to have sperm test or sperm test price Just call the Istanbul Laboratories call center (444 7 522).
Şişli Sperm Test Center: 02126311031
Kadıköy Sperm Test Center: 02166021010
instagram: labistanbul